General Dentistry
General Dentistry
Prevention is key to lifelong dental health. But know that it’s never too late to get the care you want and need.
At The National Implant Centre we provide comprehensive and minimally-invasive general dentistry services to prevent, diagnose, and solve common dental problems.
Through comfortable, advanced, modern care, our highly professional team and the National Implant Centre will ensure your pain is relieved, problems resolved, and the health and appearance of your smile improved.
We provide each patient with a personalised treatment plan based on the results of your routine exam. This details all treatments required and the prices involved. Here at the National Implant Centre we want our patients to know exactly what they need to plan for financially.

What does a routine exam involve?
- Evaluate your overall health and oral hygiene including:
- Examination of oral tissues for oral cancers
- Periodontal screening to check for gum disease
- Take a full dental base chart of your teeth
- Assess your need for tooth restoration or tooth replacement
- Occlusal examination to check for Joint / TMJ dysfunction
- Take dental X-rays or, if necessary, do other diagnostic procedures such as CT scan
- Create a customised treatment plan listing any treatments required and relevant costs involved
What is a filling?
 Dental Fillings are used to replace the parts of the tooth that have been lost, due to a number of reasons. These include wear and tear, decay and accidental damage.
Dental Fillings are used to replace the parts of the tooth that have been lost, due to a number of reasons. These include wear and tear, decay and accidental damage.
Our team uses several different kinds of fillings available such as composite (white fillings), porcelain (inlays and onlays), and amalgam (silver).
- Composite (white) fillings are made from tooth coloured resins which are very aesthetic and can be easily colour matched to your own natural dentition.
- Porcelain fillings are made by a dental technician in a laboratory and then bonded to the tooth. They can be matched to the colour of the tooth and resist staining. A porcelain restoration generally covers most of the tooth.
- Amalgam (silver) fillings are made from an amalgamation of different metals and are silver in appearance. Amalgam fillings are resistant to wear, although due to their colour, they are more noticeable than composite fillings. As such, they tend not to be used in very visible areas, such as the front teeth. It is worth noting that amalgam fillings are being phased out due to their impact on the environment.
We will take you through the pros and cons of each filling type and help you to decide which we feel is the most appropriate option to meet your clinical need.
What is Root Canal Treatment?
 Root canals are tooth-saving procedures. Root canal treatment or endodontic treatment is required when the inside of the tooth (pulp) becomes damaged or infected. This can be as a result of cracking, decay or trauma. Root canal treatments can save a tooth that is badly damaged or decayed. The treatment involves the pulp of the tooth being removed and the cavity sealed. Consequently, the tooth is restored.
Root canals are tooth-saving procedures. Root canal treatment or endodontic treatment is required when the inside of the tooth (pulp) becomes damaged or infected. This can be as a result of cracking, decay or trauma. Root canal treatments can save a tooth that is badly damaged or decayed. The treatment involves the pulp of the tooth being removed and the cavity sealed. Consequently, the tooth is restored.
How do I know if I need a root canal?
- Sensitivity to hot or cold food or drinks
- Pain when biting or chewing
- Swelling of the gum near the affected tooth
- Facial swelling
The aim of a root canal treatment is to save the tooth and prevent it from future infection. If RCT is not carried out, the infection may spread and the tooth may need to be extracted.
What is involved in root canal treatment?
Your dentist will:
- Remove the infected or damaged tissue inside the tooth
- Clean and disinfect the area
- Fill and seal the space
Depending on the strength of the remaining tooth structure after the treatment, the tooth will require either a filling or a lab made restoration.
A night guard may be recommended by your dentist to treat teeth grinding or bruxism. This is usually a plastic appliance that is worn at night time. You may be unaware that you grind your teeth or you may be having some facial/tooth pain or head-aches. Most people grind their teeth while sleeping. It is not until your dentist tells you or possibly your partner hears you grind at night that you are aware of it.
Grinding (or bruxism) can damage your teeth by causing fractures or chipping. It can also be responsible for significant jaw pain (TMJ -temporomandibular joint pain) and migraine.
These appliances even out the pressure across your jaw and create a physical barrier between your upper and lower teeth to protect them from further damage
 At the National Implant Centre we strongly advise our patients to wear a professionally made mouthguard whenever they play any sport that involves physical contact or moving objects, to significantly reduce the risk of dental injury. These offer the best protection and level of comfort for your mouth.
At the National Implant Centre we strongly advise our patients to wear a professionally made mouthguard whenever they play any sport that involves physical contact or moving objects, to significantly reduce the risk of dental injury. These offer the best protection and level of comfort for your mouth.
Most sports administrations now insist on the compulsory wearing of a mouthguard in or-der to participate.
Here at the National Implant Centre we can provide you with a specially made personal-ised mouthguard.
Our mouthguards can be made in your club or school colours if you so wish. We can al-so have your name inscribed on them so that you are less likely to ever lose it!
At the National Implant Centre, our clinic also specializes in dental emergencies. From knocked out teeth to bleeding gums, our team will get you relief. We understand the importance of urgent dental care. We strive to treat you as soon as possible and get you in and out quickly. We’re conveniently located in the heart of Ballincollig and we will take the best care of you in times of trouble.
What is an extraction?
 An extraction is the Removal of a tooth or teeth from the dental alveolar (jaw) bone.
An extraction is the Removal of a tooth or teeth from the dental alveolar (jaw) bone.
Why have an extraction?
There are generally two reasons why a Tooth is removed;
- When the tooth is damaged beyond reasonable repair.
- When the tooth is not well positioned or is non functional.
Extensively decayed, cracked or badly broken teeth are usually best removed. The conditions that warranted extraction are usually so extreme that regular reconstructive work (e.g fillings, crowns etc) will not be effective.
Sometimes teeth need to be extracted if the gums are badly damaged as a result of periodontal disease. gum disease affects THE supporting bone or foundations of a tooth resulting in the tooth becoming very loose. Inhibiting function or causing pain.
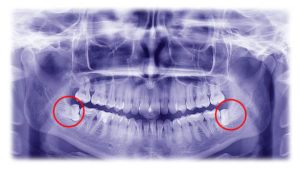
On occasion, the extraction of a healthy tooth is indicated it is badly positioned. Badly positioned teeth can affect oral hygiene as they can be difficult to access and therefore can cause pain and irritation. These teeth may need to be removed to improve oral hygiene and/or prevent compromising adjacent teeth. Wisdom teeth can often fall into this category. The wisdom teeth are at the back of the mouth and can be difficult to clean and maintain. Improper cleaning can lead to cavities, tooth decay and gum disease. Sometimes it is best to remove the wisdom teeth as a preventative measure against future problems. Many times wisdom teeth are LODGED or impacted in awkward positions so they emerge from the gum at unusual angles.
How is an extraction done?
Generally, an x-ray is taken prior to the extraction of a tooth. This picture gives the dentist information as to the best way to remove a tooth. Next, local anesthetic is administered so that the extraction is comfortable and pain free for the patient. Many patients experience some degree of pressure on the tooth during the procedure. Sometimes, teeth are firmly rooted and we may need to remove them in sections. The patient is generally informed of this prior to the procedure. Once the tooth is removed, the patient bites down on a damp-ened cotton swab to help the blood in the area clot. After every extraction, a patient is ad-vised of the risks of pain, bruising and swelling.
Aftercare Instructions
For the first 24 hours after your dental surgery you should avoid;
- Any food or drinks that are very hot or cold.
- Mouth washes
- Smoking
- Alcohol
- Exercise
As these can all cause post-operative BLEEDING (hot drinks are allowed as long as they have been allowed to cool to warm).
Avoid any food that is sharp, scratchy or sticky (e.g toffee or chewing gum). WE ADVISE STICKING TO A SOFT Diet for the first 48 hours following your surgery.
Local anaesthesia:
During your surgery today you may have been given an injection of local anesthesia in the gum near where your tooth has been extracted or had a surgical procedure. This helps to minimise any pain after the operation. This ANAESTHETIC also causes temporary numbness to areas inside your mouth. Be careful not to chew the insides of your cheeks or accidentally bite your lips or tongue. The local anaesthetic will gradually wear off over the next few hours but you may experience a slight loss of sensation on patches of skin for a short period after surgery.
Bleeding:
Bleeding should stop soon after your surgery you may find the sockets ooze slightly for 24 hours. You will receive a supply of dental packs to take home. If bleeding persists, apply the pack over the bleeding socket and bite firmly for 20 minutes. If after 20 minutes the bleeding continues, please contact us.
If you don’t have one of the dental packs to hand, then use a clean handkerchief rolled up so that one corner is made into a hard pad twice the size of the bleeding socket.
Once the bleeding has stopped a blood clot will form over the socket. It is important to try not to knock that blood clot away or you may cause the socket to start bleeding again.
Mouthwashes:
Mouthwashes should be started 24 hours after your surgery. Mix a level teaspoon of salt into a cup of boiled, hot(but not scalding) water. Hold the salt water in your mouth for one minute and gently swish around and then spit out. Repeat 3-4 times a day and after you have EATEN to make sure your mouth remains clean. Do not use any other mouthwashes, unless directed, after the surgery. Tooth brushing should continue as normal.
If you notice an unpleasant taste, smell or discharge, it may indicate an infection, please contact us if concerned.
Pain Relief:
During the week following your surgery, you may experience some discomfort, swelling and bruising around your cheeks jawline and neck. Due to the inflammation around the joint your jaw may also become stiff. With time and regular use of painkillers this should subside. Alternative therapies, such as a warm wheat pack placed around the neck or a bag of frozen peas wrapped in a tea towel applied to the jaw may help.
Stitches:
If any stitches have been used these stitches will be disposable unless you are told otherwise. The stitches will dissolve in approx 10 days -2 weeks. Do not fiddle with the stitches with fingers or tongue. It is ADVISABLE to continue with warm salted water until stitches dissolve.
